Understanding Fissure Surgery: Treatment and Recovery.
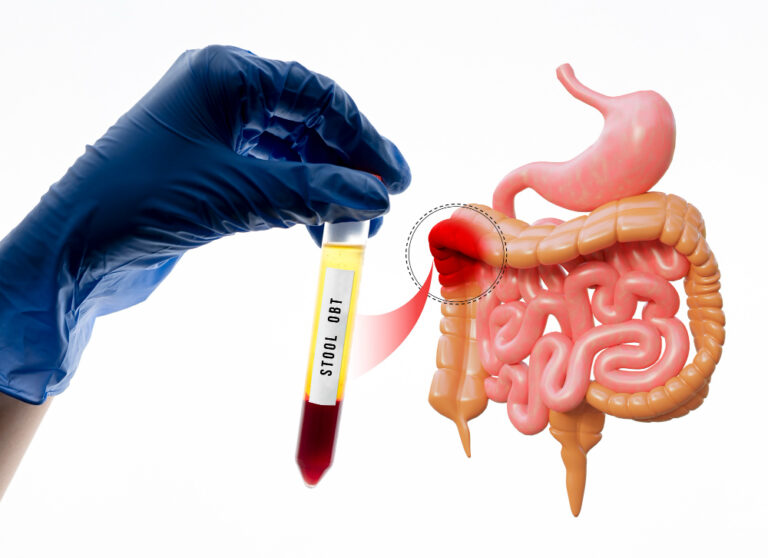
An anal fissure is a common and often painful condition characterized by a small tear or cut in the lining of the anus. While many fissures can heal with conservative treatments like dietary changes and topical ointments, some cases may require surgical intervention. This article aims to explore the specifics of fissure surgery, including when it’s necessary, what to expect during the procedure, and how to navigate recovery effectively.
To Know More About It Please Click Here
When is Fissure Surgery Necessary?
Fissure surgery is typically considered when conservative treatments have not effectively resolved the fissure or when the fissure becomes chronic (lasting longer than 6 weeks) and causes persistent pain or bleeding. The decision to proceed with surgery is often made by a colorectal surgeon after evaluating the severity and duration of the fissure and considering the patient’s overall health and lifestyle factors.
Types of Fissure Surgery
There are several surgical options available for treating anal fissures. The choice of procedure depends on the specific characteristics of the fissure and the surgeon’s preference. Common surgical interventions include:
- Lateral Internal Sphincterotomy (LIS): This is the most common surgical procedure for chronic anal fissures. It involves cutting a small portion of the internal anal sphincter muscle to reduce spasm and promote healing of the fissure. By relaxing the sphincter, blood flow to the fissure increases, aiding in the healing process.
- Fissurectomy: In this procedure, the surgeon removes the entire fissure or the scar tissue around it. This approach may be suitable for certain types of fissures or when a sphincterotomy is not preferred.
- Botulinum Toxin Injection: Although not technically surgery, injecting botulinum toxin (Botox) into the anal sphincter can help relax the muscle and promote healing in some cases of chronic fissures.
What to Expect During Fissure Surgery
Fissure surgery is usually performed as an outpatient procedure under local anesthesia or sedation. The surgery itself is relatively quick, typically lasting less than 30 minutes. Here’s what you can expect:
- Preparation: You may be asked to fast for a few hours before the procedure.
- Anesthesia: Local anesthesia is administered to numb the area around the anus.
- Procedure: The surgeon performs the chosen surgical technique (e.g., sphincterotomy or fissurectomy).
- Recovery: After the procedure, you will be monitored briefly in a recovery area before being discharged home.
Recovery and Aftercare
Recovery from fissure surgery varies depending on the type of procedure performed but generally involves the following:
- Pain Management: Mild discomfort and some bleeding are common after surgery. Your doctor may prescribe pain medications or recommend over-the-counter options.
- Stool Softeners: To prevent straining during bowel movements, your doctor may recommend using stool softeners or fiber supplements.
- Hygiene: Keep the anal area clean and dry. Sitz baths (sitting in warm water) can help relieve discomfort and promote healing.
- Follow-Up: Attend all scheduled follow-up appointments to monitor healing and address any concerns.
Potential Risks and Complications
While fissure surgery is generally safe, like any surgical procedure, it carries some risks, including infection, bleeding, and recurrence of the fissure. It’s essential to follow your doctor’s post-operative instructions carefully to minimize these risks.
To Know More About It Please Click Here
Final Thoughts
Fissure surgery can provide relief for individuals suffering from chronic anal fissures that do not respond to conservative treatments. By understanding the procedure, preparing appropriately, and following post-operative care instructions diligently, patients can optimize their recovery and improve their quality of life. Always consult with a qualified colorectal surgeon to discuss the best treatment options for your specific condition.