Advancements In Pilonidal Sinus Surgery: Emerging Techniques And Technologies
Pilonidal sinus, a common condition characterized by the development of an abnormal tract or tunnel in the skin near the tailbone, often requires surgical intervention for resolution. Over the years, significant advancements have been made in the field of pilonidal sinus surgery, with emerging techniques and technologies aiming to improve outcomes, minimize complications, and enhance patient satisfaction. This article explores the latest innovations in pilonidal sinus surgery, highlighting their potential benefits and implications for patient care.
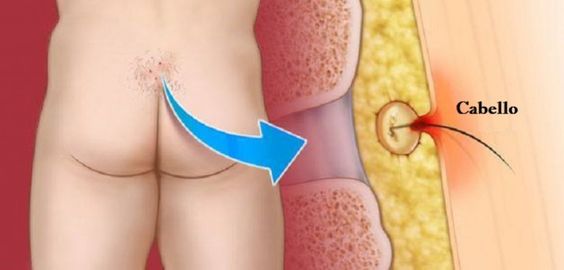
Understanding Pilonidal Sinus
Before delving into advancements in surgery, it’s crucial to understand the nature of the pilonidal sinus. This condition typically arises from hair follicles becoming embedded in the skin, leading to the formation of a sinus tract prone to infection and inflammation. Pilonidal sinus can cause pain, swelling, drainage of pus, and recurrent abscesses, significantly impacting patients’ quality of life.
Traditional Surgical Approaches
Historically, surgical excision with primary closure or open wound healing has been the mainstay of treatment for pilonidal sinus. While effective, these approaches are associated with drawbacks such as prolonged healing times, high rates of recurrence, and potential complications like wound infections and delayed wound closure. As a result, there has been a growing interest in exploring alternative techniques and technologies to address these challenges.
Emerging Techniques and Technologies
Minimally Invasive Surgery:
One of the most significant advancements in pilonidal sinus surgery is the adoption of minimally invasive techniques. Procedures such as minimally invasive pilonidal sinus surgery (MIPSS) or endoscopic pilonidal sinus treatment (EPSiT) utilize small incisions and specialized instruments to access and remove the sinus tract while preserving surrounding tissue. Minimally invasive approaches offer several advantages, including reduced postoperative pain, faster recovery, and improved cosmetic outcomes compared to traditional open surgery.
Laser Therapy:
Laser therapy has emerged as a promising adjunctive treatment for pilonidal sinus. Laser ablation involves the targeted application of laser energy to destroy the sinus tract and surrounding tissue, promoting wound healing and reducing the risk of recurrence. Laser therapy is minimally invasive, requires shorter procedure times, and can be performed under local anesthesia in an outpatient setting. Additionally, laser therapy may offer advantages in terms of reduced pain and faster return to normal activities compared to conventional surgery.
Biological and Synthetic Scaffolds:
Another area of innovation in pilonidal sinus surgery involves the use of biological and synthetic scaffolds to support tissue regeneration and wound healing. These scaffolds, composed of materials such as collagen, hyaluronic acid, or synthetic polymers, are placed within the surgical site to promote tissue ingrowth and facilitate wound closure. By providing a scaffold for cell proliferation and migration, these materials can enhance the healing process and reduce the risk of recurrence following surgery.
Negative Pressure Wound Therapy (NPWT):
Negative pressure wound therapy, commonly known as vacuum-assisted closure (VAC), has been increasingly utilized in the management of complex wounds, including pilonidal sinus defects. NPWT involves the application of controlled negative pressure to the wound bed, promoting tissue perfusion, reducing edema, and facilitating wound contraction. In pilonidal sinus surgery, NPWT can help optimize wound healing, minimize wound complications, and accelerate the closure of large or contaminated wounds.
Surgical Sealants and Adhesives:
Surgical sealants and adhesives offer an alternative approach to traditional sutures or staples for wound closure in pilonidal sinus surgery. These products, which may include cyanoacrylate-based adhesives or fibrin sealants, provide a seal over the wound site, preventing fluid leakage and minimizing the risk of infection. Additionally, surgical sealants can help reinforce tissue apposition, reduce tension on the wound edges, and promote faster healing compared to conventional closure methods.
Conclusion
Advancements in pilonidal sinus surgery, including emerging techniques and technologies, hold promise for improving patient outcomes and enhancing the overall surgical experience. Minimally invasive approaches, laser therapy, biological and synthetic scaffolds, negative pressure wound therapy, and surgical sealants represent innovative strategies aimed at addressing the limitations of traditional surgical methods. As these advancements continue to evolve and gain acceptance, they have the potential to revolutionize the management of pilonidal sinus, offering patients more effective, efficient, and minimally invasive treatment options.