Laser Therapy For Hydrocele: An Emerging Trend In Surgical Innovation
Hydrocele, a common condition characterized by the accumulation of fluid around the testicles, has traditionally been treated through surgical procedures such as hydrocelectomy. However, recent advancements in medical technology have led to the emergence of laser therapy as a promising alternative in the treatment of hydrocele. This article explores the principles behind laser therapy for hydrocele, its potential advantages, the procedure itself, and the current status of this innovative approach in urological surgery.
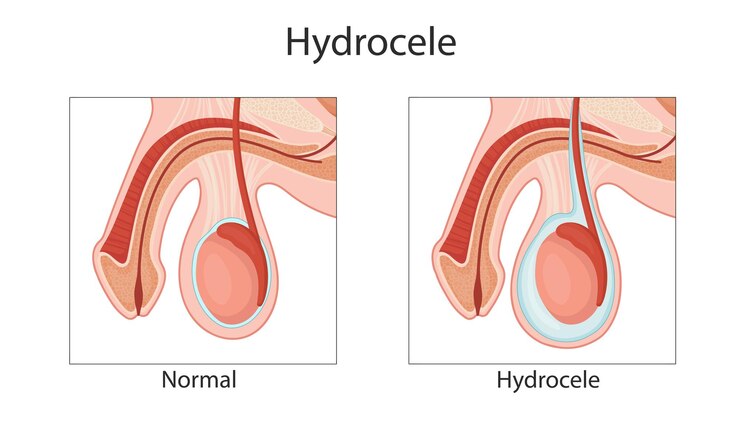
Understanding Hydrocele and Conventional Treatments
Before delving into laser therapy, it’s essential to understand hydrocele and the traditional treatment options available. A hydrocele occurs when excess fluid collects in the sac surrounding the testes, leading to swelling and discomfort. Conventional treatments for hydrocele include watchful waiting, drainage procedures, and hydrocelectomy – a surgical intervention where the accumulated fluid is drained, and the sac is either removed or modified to prevent fluid re-accumulation.
The Emergence of Laser Therapy
Laser therapy for hydrocele represents a significant advancement in the field of urological surgery. This innovative approach utilizes laser energy to target and seal the blood vessels that contribute to the formation of fluid within the sac. The idea behind laser therapy is to achieve a minimally invasive procedure that reduces trauma, promotes faster recovery, and potentially lowers the risk of complications associated with traditional surgery.
Advantages of Laser Therapy for Hydrocele
Minimally Invasive Nature:
Laser therapy for hydrocele is considered a minimally invasive procedure, involving small incisions or punctures rather than large surgical cuts. This results in less tissue damage, reduced pain, and a quicker recovery time compared to conventional hydrocelectomy.
Precision and Control:
Lasers provide surgeons with a high degree of precision and control during the procedure. This allows for targeted treatment, minimizing damage to surrounding tissues and structures, and potentially reducing the risk of complications.
Reduced Bleeding:
Laser therapy is associated with reduced intraoperative bleeding due to the coagulative properties of laser energy. This can contribute to a clearer surgical field, making the procedure more efficient and safer.
Faster Recovery:
Patients undergoing laser therapy for hydrocele may experience a faster recovery compared to traditional surgical approaches. The minimally invasive nature of the procedure and reduced tissue trauma contribute to quicker healing and a shorter hospital stay.
Lower Infection Risk:
With smaller incisions and less tissue manipulation, the risk of postoperative infections may be lower in laser therapy for hydrocele compared to traditional surgery.
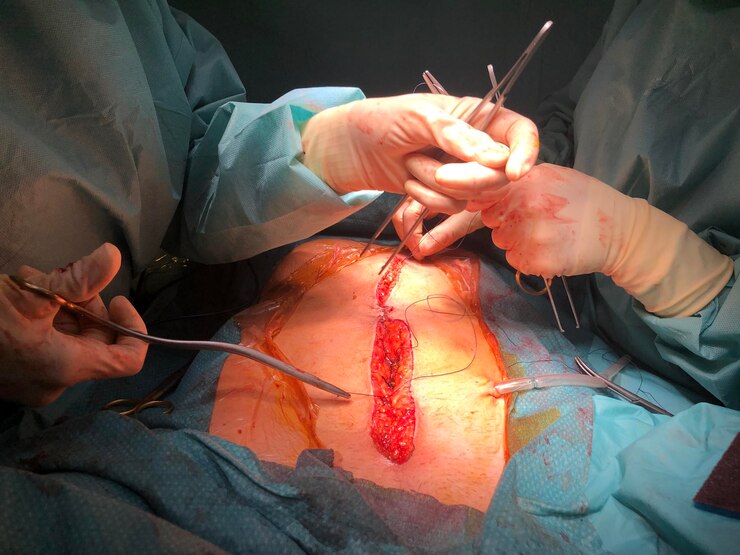
The Laser Therapy Procedure
The laser therapy procedure for hydrocele involves several key steps:
Anesthesia:
The patient is typically given local or regional anesthesia to numb the surgical area. In some cases, general anesthesia may be used.
Incision or Puncture:
Small incisions or punctures are made to access the hydrocele sac. The use of lasers allows for precision in creating these openings.
Laser Application:
Laser energy is then applied to the blood vessels within the sac. The laser’s coagulative properties help seal the vessels, preventing the accumulation of fluid.
Closure:
Once the laser therapy is complete, the incisions or punctures are closed using sutures or adhesive strips.
Recovery:
Patients are monitored postoperatively, and most can expect to return home on the same day. Recovery time is generally shorter than that associated with traditional hydrocelectomy.
Current Status and Future Directions
While laser therapy for hydrocele shows promise as an emerging trend in surgical innovation, it is essential to note that research on its long-term efficacy and outcomes is still in the early stages. Current studies suggest favorable short-term results, including reduced postoperative pain and quicker recovery, but more extensive research is needed to establish its effectiveness over the long term.
The use of laser therapy for hydrocele is also dependent on factors such as the size of the hydrocele, patient preferences, and the surgeon’s expertise. As the technique evolves and more data becomes available, it is likely that laser therapy will find a place in the broader spectrum of hydrocele treatment options.
Conclusion
Laser therapy for hydrocele represents a promising advancement in the field of urological surgery. With its minimally invasive nature, precision, and potential for faster recovery, it offers an alternative to traditional hydrocelectomy. While the procedure is still undergoing further research to establish its long-term efficacy, the initial results are encouraging.
As technology continues to advance, laser therapy for hydrocele may become more widely adopted, offering patients a less invasive and more efficient option for addressing this common urological condition. Close collaboration between urologists, researchers, and technology developers will play a crucial role in shaping the future of hydrocele treatment and ensuring that patients benefit from the latest innovations in surgical care.